All families will come into contact with the NHS at some point for healthcare, but if your child has a disability or health condition then you may find you use lots of different services provided by the NHS and have more frequent contact with health professionals.
On this page, you may find some pointers and organisations that may help you, your child/young person or your family when it comes to healthcare for those with Special Educational Needs and Disabilities.
Download Full Document booklet

Table of Contents
Youtube Video
Feedback
Once you have completed the workshop, please take a few minutes to fill in the below feedback form.
The 3 Levels of Care within the Health System
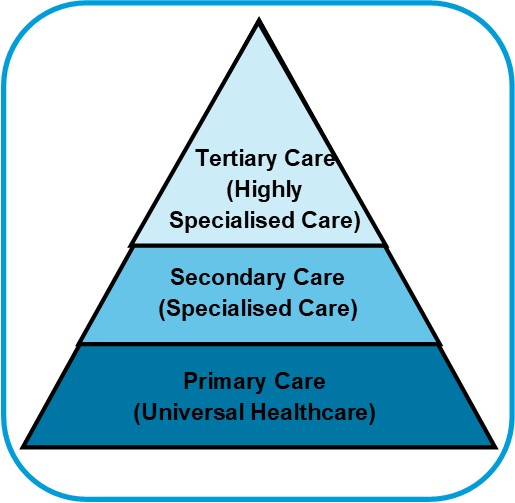
Primary Care
This is universal healthcare provided for a local community that is accessed directly. Examples include:
- GP
- Dentist
- Opticians
- Practice Nurse
- Pharmacy
Primary Care is commissioned by NHS England, School Nursing is commissioned by the Local Authority and A&E services are commissioned by your local Clinical Commissioning Group.
Secondary Care
This is more specialised healthcare that requires a referral from primary care to access. In most cases your GP will be responsible for providing a referral to a secondary health care professional. This secondary care maybe based in a community health setting or a local hospital. Some examples include:
- Community Paediatricians
- Occupational Therapists
- Physiotherapists
- Speech & Language Therapists
- Audiologists
- Child Adolescent & Mental Health Services (CAMHS)
Most secondary health services will be commissioned by the local Clinical Commissioning Group (CCG).
Tertiary Care
This is highly specialised healthcare services that requires a referral from primary or secondary care, normally this will be your GP or community paediatrician, but may include other secondary health professionals. Examples include:
- Consultant Paediatrician (Specialist Hospital)
- Specialist Nursing Teams
- Child Adolescent and Mental Health Services (CAMHS)
Specialist Tertiary services are commissioned by NHS England.
Consent to Treatment
Before a medical practitioner can examine or treat your child, they need consent. The way consent is asked for partly depends on what the medical practitioner plans to do.
If a GP wishes to look in your child’s throat they will ask your child to open their mouth. You may then need to encourage your child to do so. This is usually enough to demonstrate that they and you have given consent. For more complex health care and treatment there are some differences in the rules about consent for children, young people and adults.
Adults
Once a person has reached the age of 18, no one can give consent on their behalf. If they are not competent, clinicians can provide treatment and care providing this is in their best interests.
The Mental Capacity Act 2005 governs decisions made on behalf of adults when they do not have mental capacity.
Young people aged 16 and 17 years
These young people are presumed to have the competence to give consent to treatment for themselves. The Department of Health recommends that it is good practice to encourage young people of this age to involve their families in decisions about their, care unless it would not be in their interests to do so.
Children under 16 years of age

Children under 16 years of age can give consent to medical treatment, providing they have demonstrated they have sufficient capacity to decide. This depends on their ability to understand what is involved in making the decision. There isn’t a general test to assess a child’s capability and each case should be assessed based on the individual circumstances. When a child is not able to give informed consent, a person with parental responsibility can give consent for them.
Patient Information and Liason Services
The Patient Information and Liaison Service (PILS) is a confidential service provided by NHS organisations including hospitals, mental health services, community services and clinical commissioning groups. They can help if you:
- don’t know what’s happening
- want information but don’t know where to get it
- would like to resolve a situation but don’t want to complain
- need to complain but not sure how
- want to speak to someone but not sure who
Website: Leicester Hospitals PILS
Phone: 0808 178 8337
Email: pils@uhl-tr.nhs.uk
Local Authority Responsibilities
Leicester’s Health and Wellbeing Board has been set up to develop and deliver joint health and wellbeing strategies through partnership working.
The SEND Code of Practice says:
Local authorities, CCGs and other partners must work together in local Health and Wellbeing Boards to assess the health needs of local people, including those with SEN or who are disabled. (1.19)
CCGs, NHS Trusts and NHS Foundation Trusts must inform the appropriate local authority if they identify a child under compulsory school age as having, or probably having, SEN or a disability (Section 23 of the Children and Families Act 2014). (1.16)
The introduction of the 2014 Care Act gave Local Authorities the legal duty to offer access to independent Advocacy to anyone engaged in adult social care processes.
The Local Authority must arrange an independent advocate to facilitate:
- The involvement of a person in their assessments
- Preparation and review of their care and support plans
- Support through safeguarding adult enquiries and reviews under the Care Act 2014
Who is Independent Care Act Advocacy for?
The service is available to anyone living in the counties of Leicestershire or Rutland for:
- Adults
- Young people going through transitions
- Care leavers
- Carers
- Young carers
- Prisoners currently detained in the area who are subject to Social Care processes and are struggling to engage with or understand the process.
Website: Care Act Advocacy Service
Phone: 0116 204 5110
Email: advocacy@ageukleics.org.uk
POhWer is a charity that provides information, advice, support and advocacy to people who experience disability, vulnerability, distress and social exclusion. The Leicester service handles NHS complaints, Independent Mental Health Advocacy and Mental Capacity Advocacy.
Website: POhWer Leicester
Phone: 0300 456 2370
Email: pohwer@pohwer.net
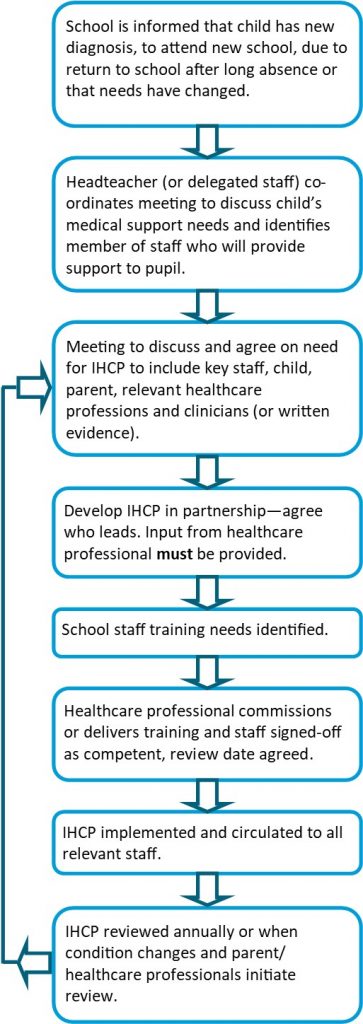
Healthcare within School and Education Settings
Every child is entitled to education. Governing bodies must ensure that arrangements are in place in schools to support pupils at school with their medical needs. School leaders should consult health and social care professional, pupils and parents to ensure that the needs of children with medical conditions are properly understood and effectively supported.
Supporting Pupils with Medical Conditions
Designated Clinical Officers (DCO’s) are the point of contact for local authorities, schools and colleges seeking health advice on children and young people who may have SEN or disabilities. They can support schools with their duties under the ‘Supporting Pupils with Medical Conditions’ guidance.
Health professionals (for example school or specialist nurses and therapists) may work directly with your child/young person and advise or train settings to manage health conditions such as epilepsy and diabetes, or with techniques such as tube feeding, in schools.
School policies should include:
- who is responsible for ensuring that sufficient staff are suitably trained;
- a commitment that all relevant staff will be made aware of the child’s condition;
- cover arrangements in case of staff absence or staff turnover to ensure someone is always available;
- briefing for supply teachers;
- risk assessments for school visits, holidays, and other school activities outside the normal timetable; and
- monitoring of individual healthcare plans
Individual Healthcare Plans
An Individual Healthcare Plan is designed to keep children with medical conditions safe, well and involved at school. They are not the same as Education, Health and Care Plans (EHCP), but some children may have both an EHCP and an Individual Healthcare Plan.
You and your child’s school should agree how often the healthcare plan will be reviewed. It’s advised that this happens at least once a year, but it may need to happen more frequently if your child’s condition is unstable or their medication changes.
Who needs an Individual Healthcare Plan?
There’s no specific guidance on what sort of medical conditions warrant an individual healthcare plan, and it’s up to schools to decide if your child needs one. If your child has a severe or complex medical problem or needs specialist care, a healthcare plan is likely to be essential, but for less complicated conditions, it may not be necessary.
Schools are advised to use common sense when deciding whether a child should have a healthcare plan, and should take your views into account. They must also consider each child’s case individually – children vary in how they cope with medical conditions, and some may need extra help to manage a condition that another child is able to handle by themselves.
What does an Individual Healthcare Plan include?
Individual healthcare plans should be as simple and uncomplicated as possible. Schools are free to draw up their own plans, and the level of detail included will depend on each child’s needs. However, a good care plan should include:
- Your child’s personal details: name, date of birth, class, and ideally a photo to help staff identify them.
- The name of their condition/s.
- Contact details for both parents or other family members, the GP and their clinic or consultant.
- A description of their condition and the symptoms that affect them.
- Information about your child’s daily care requirements: for instance medication (including dose, storage requirements and side effects), dietary requirements, special facilities needed in school (such as access to a disabled toilet), and social and environmental needs (such as extra time between lessons).
- What sort of support your child needs with their daily care, and who at school will administer it.
- What constitutes a medical emergency relating to your child’s condition, and what action they should take if it occurs – for example, administering an epipen in the event of an anaphylactic reaction.
- The date of preparation of the plan, and the date when it should be reviewed.
If your child will need to be given medication at school, you should also be asked to fill in a form giving details of their treatment and your permission for staff members to administer it (or for your child to take it themselves, if they are old enough and able to do so).
Equality and Inclusion
Some children may not be able to attend school for health reasons, for long term or intermittent periods.
For children with SEND, anxiety or sensory overload are common factors affecting attendance, which are sometimes not immediately identified. If you think there may be underlying needs affecting your child’s attendance, discuss and explore with school how these might be supported.
A reduced timetable can be an effective temporary measure to support some children. There should be a plan to support an increase to full-time, regular reviews and only with parental agreement and involvement of appropriate services.
If you are feeling pressured to accept a reduced timetable, talk to school about whether there are other appropriate support options, for example:
- A Common Assessment Framework (CAF), which is a shared assessment and planning framework.
- Referral for Alternate Provision (such as the Children’s Hospital School or a Pupil Referral Unit)
- Referral to a health service (such as CAMHS)
- Where support options in school have been exhausted, a request to the local authority to carry out an EHC needs assessment
- where an EHC plan is already in place, requesting an early annual review

The Department for Education Guidance about Attendance says:
“All pupils of compulsory school age are entitled to a full-time education. In very exceptional circumstances there may be a need for a temporary part-time timetable to meet a pupil’s individual needs. A part-time timetable must not be treated as a long-term solution. Any pastoral support programme or other agreement must have a time limit by which point the pupil is expected to attend full-time or be provided with alternative provision.”
Unacceptable Practices
Many parents report that they are being asked to come into school to attend to their child or are facing action over the poor attendance of a sick child. The guidance lists a number of practices that are considered unacceptable, for example:
- Asking parents to come in to give medication or attend to toileting.
- Ignoring the views of children, parents and medical professionals.
- Sending children home unnecessarily.
- Penalising pupils who are absent for medical reasons.
- Assuming that all children with the same condition require the same treatment.
- Preventing access to medication.
- Stopping children from eating or taking toilet breaks where this is necessary.
- Putting barriers in the way of children taking part in all aspects of school life including trips.
Getting the right help in place

It’s important to notify the school as soon as your child is diagnosed with a medical condition. If your child is about to start or change school, try to work with the new school in advance so the right support can be put in place from the beginning. Ask for the school’s medical needs policy and ask for a meeting with the member of staff responsible for medical needs.

Frequently Asked Questions
My child has medical needs. Can she/he have an Education, Health and Care (EHC) plan?
Although EHC plans cover all three areas, including health, they are education driven. It is only possible to trigger the EHC assessment process if your child has an educational need. However it is worth bearing in mind that the definition of special educational need has two parts and includes:
- Children who have significantly greater difficulty in learning than others of their age.
- Children with a disability who can’t access educational facilities normally available in mainstream school.
Some children with medical needs may fit the disability part of the definition.
We have more information on Education, Health and Care Plans on our website. You can also contact us for guidance.
Can school staff refuse to give my child medication?
Giving medication is not part of schoolteachers’ conditions of service, so an individual teacher can’t be forced to give medication. Teachers can volunteer to do so if they wish. Support staff may have the requirement to give medicine written into their contract.
The school should ensure that there are sufficient trained staff available to give medication to children who cannot manage it themselves. Parents should not be asked to come into school to give medication.
Can health and social care provision be written in to an EHC plan?
It is important to note that health care provision or social care provision which educates or trains a child or young person is treated as special educational provision (section 21(5) of the Children and Families Act 2014). A good example of this is speech therapy. It looks like it should be health provision – because it is usually provided by the Health Service – but it must be treated as special educational provision. This is because speech and language therapy “educates or trains” a child or young person to communicate more effectively.
Any health care provision will have to be agreed by the local Clinical Commissioning Group (“CCG”) before it can be written into an EHC plan. Once provision is written in to an EHC plan, it is legally enforceable. If it is in the education or social care provision sections of the EHC plan, then the Local Authority (LA) must ensure it is provided. If it is in the health care provision section, then the CCG must provide it.
What if the health and social care provision in the EHC plan is inaccurate or inadequate?
During an EHC needs assessment, the LA should seek advice and information from health and social care. If this is not done, this could lead to inaccurate or inadequate sections of the EHC plan, which are blank, or say “not known to the service” or “no health/social care needs” when this is not the case.
Leicester & Leicestershire Based Organisations:
Clasp the Carers Centre
 Leicestershire based charity, dedicated to supporting family carers who look after people with different needs. The Carers Centre is here to support all unpaid carers to understand what their rights and entitlements are and how they can access services to help them with their caring role.
Leicestershire based charity, dedicated to supporting family carers who look after people with different needs. The Carers Centre is here to support all unpaid carers to understand what their rights and entitlements are and how they can access services to help them with their caring role.
Website: Clasp the Carers Centre Website
Phone: 0116 251 0999
Email: enquiries@thecarerscentre.org.uk
Early Intervention Service

The service is a partnership of organisations –Relate, ADHD Solutions and Centre for Fun and Families. The service supports children and young people who present with low level mental health needs, which impact on their daily lives but do not meet the Children and Adolescent Mental Health Service (CAMHS) criteria and cannot be supported by universal services. For example, children who suffer from:
- Low mood
- Self-harm
- Anger management issues
- Anxiety
- Academic stress and school transitions
- Family relationships issues
- Coping with their illness or someone close
- Bullying (including social media)
- Loneliness and rural isolation
Professionals work in partnership to deliver counselling and group work for children, young people and parents. Children & Young People who do not meet the criteria for the service will be referred to an appropriate service.
Referral to the Early Intervention Service comes from GPs and CAMHS.
Phone: 0116 254 3011
Email: Reception@rllr.org.uk
Healthwatch Leicester

Healthwatch is set up to champion the views of patients and social care users in Leicester and Leicestershire, with the goal of making services better and improving health and wellbeing. They want to hear about your views, needs and experiences to help Leicester and Leicestershire get the best possible health and care.
Website: Healthwatch Leicester
Phone:0116 251 8313
Email: enquiries@healthwatchll.com
Leicester Carers Support Service
![]() If you look after a friend or family member, who relies on your support to manage their daily life, you are a Carer. The Leicester Carers Support Service can offer free and confidential support and we are here to help you.
If you look after a friend or family member, who relies on your support to manage their daily life, you are a Carer. The Leicester Carers Support Service can offer free and confidential support and we are here to help you.
Website: Leicester Carers Support Service
Phone: 0116 222 0538
Email: carers@ageukleics.org.uk
Leicester City Disabled Children’s Services
 Support for disabled children, young people and their families ran by the council. This includes activities, support and services available to families, Preparing for Adulthood, Personal Assistants, Short Breaks, and more.
Support for disabled children, young people and their families ran by the council. This includes activities, support and services available to families, Preparing for Adulthood, Personal Assistants, Short Breaks, and more.
Website: Disabled Children's Services
Phone: 0116 454 1004
Leicester City Early Help

The early help offer brings together a range of services to support children, young people and their families who need some additional help.
Website: Early Help Website
Phone: 0116 454 1004
Email: early-help@leicester.gov.uk
Leicester Local Offer
 Information and guidance that can support children and young people with SEND, aged 0 to 25, in Leicester. Every Local Authority has a legal duty to provide this service.
Information and guidance that can support children and young people with SEND, aged 0 to 25, in Leicester. Every Local Authority has a legal duty to provide this service.
Website: Leicester Local Offer
Parent Carer Forum

They engage with Parent Carers, the Local Authority, Health Services, Special Education Services, Disabled Children's Services, and the Voluntary Sector to co-produce, develop, improve and scrutinise the City's SEND services.
Website: Leicester City Parent Carer Forum (LCPCF)
Phone: 07455 745344
Email: info@lcpcf.net
National Organisations:
Contact A Family

Contact support families with the best possible guidance and information. They bring families together in local groups and online, to support each other by sharing experiences and advice. And they help families to campaign, volunteer, fundraise and shape local services to improve life for themselves and others.
Website: Contact a Family
Phone: 020 7608 8700
Email: info@contact.org.uk
Council for Disabled Children

The umbrella body for the disabled children's sector bringing together professionals, practitioners and policy-makers. Their website has a variety of information, help sheets and links to other organisations.
Website: Council for Disabled Children
Email: cdc@ncb.org.uk
Health for Under 5's
 Health for under 5s was developed by professionals working for Leicestershire Partnership NHS Trust (LPT), with support from Leicester City Council, Leicestershire County Council and Rutland County Council.
Health for under 5s was developed by professionals working for Leicestershire Partnership NHS Trust (LPT), with support from Leicester City Council, Leicestershire County Council and Rutland County Council.
This website has been produced specifically for prospective parents as well as parents and carers of children from 0-5 years. It contains information to support you during those initial formative years.
The information provided is concise, clear and easy to understand, with the tone of having a ‘chat’ with your health visitor. The content is therefore conversational and avoids the use of detailed medical terminology wherever possible.
Website: Health for Under 5's
Text: 07520 615381
Health for Kids

Health for Kids: Grownups is specifically for parents and carers of primary school aged children.
This website contains information to support you during a child’s primary school years.
The information provided is concise, clear and easy to understand. The content is therefore conversational and avoids the use of detailed medical terminology wherever possible.
There is also the Health for Kids: Kids section of the website to include your child in the discussions around health.
Website: Health for Kids
Health for Teens
 Health for Teens introduces a new and different way for young people aged 11-19 to learn about their health. This website features bite-sized information on a comprehensive range of physical and emotional health topics for teenagers, including healthy eating, body image, managing stress, advice on relationships, puberty, sexuality and much more. Movie clips and quizzes make the site engaging and interactive, and young people are able to share content easily with their peers via social media.
Health for Teens introduces a new and different way for young people aged 11-19 to learn about their health. This website features bite-sized information on a comprehensive range of physical and emotional health topics for teenagers, including healthy eating, body image, managing stress, advice on relationships, puberty, sexuality and much more. Movie clips and quizzes make the site engaging and interactive, and young people are able to share content easily with their peers via social media.
Website: Health for Teens
Mencap

Mencap are here to improve the lives of people with a learning disability and their families.
Website: Mencap
Helpline: 0808 808 1111
Helpline Email: helpline@mencap.org.uk
NHS: Children & Young People's Services

Information about what to do if you are concerned about your child.
Website: NHS Children & Young People's Services
Scope

Disability equality charity in England and Wales that provide practical information and emotional support to families.
Website: Scope
Helpline: 0808 800 3333
Helpline Email: helpline@scope.org.uk
